The new integrated plans are intended to allow better coordination of services and to make the system easier. Managed care also called managed health care type of health insurance and system of delivering health care services that is intended to minimize costs.
A MCO is an insurance company contracted to perform the management and administration of programs or services for the state.

Managed care programs. These providers make up the plans network. If the primary care doctor makes a referral outside of the network of providers the plan pays all or most of the bill. Managed care is specific to health care in the United States.
Managed Care Programs The Health and Human Services Commission has transitioned certain programs and services to Managed Care Organizations MCO. Three different types of arrangements are commonly referred to as managed care within the Medicaid policy arena. Health Maintenance Organizations HMOs Preferred Provider Organizations PPOs and Point of Service POS plans.
Once approved Managed Care members get their health care services through the MO HealthNet Managed Care health plan of their choice. The Health Plan you choose will offer you a full range of. When you enroll in managed care you become a member of a Health Plan.
Managed care organizations negotiate with providers to provide services to their enrollees either on a fee-for-service basis or through arrangements under which they pay providers a fixed periodic amount to provide services. Medi-Cal Managed Care contracts for health care services through established networks of organized systems of care which emphasize primary and preventive care. If the state program requires MCO Accreditation Requirements.
You will have at least 5 Health Plans to choose from depending on where you live. A POS plan allows members to refer themselves outside the HMO network and still get some coverage. They have contracts with health care providers and medical facilities to provide care for members at reduced costs.
Managed Care is a term that is used to describe a health insurance plan or health care system that coordinates the provision quality and cost of care for its enrolled members. Managed care organizations MCOs are rapidly becoming a major source of health care for the beneficiaries of both employer-funded care and of the publicly funded programs Medicaid and Medicare. In addition MCOs represent organized care systems that often focus their efforts on defined populations and are accountable for desired outcomes.
How much of your care the plan will pay for depends on the networks rules. The MO HealthNet Managed Care Program can help pay for qualified medical costs for some people with limited income and resources. Comprehensive risk-based plans are the most commonly used type of Medicaid managed care arrangement.
A POS managed care plan is offered an option within many HMO plans. Make sure to address the following areas. Managed care is a kind of health insurance program.
Managed care plans are a type of health insurance. The origins of managed care in the United States can be traced to the late 19th century when a small number of physicians in several US. Managed care program integrity.
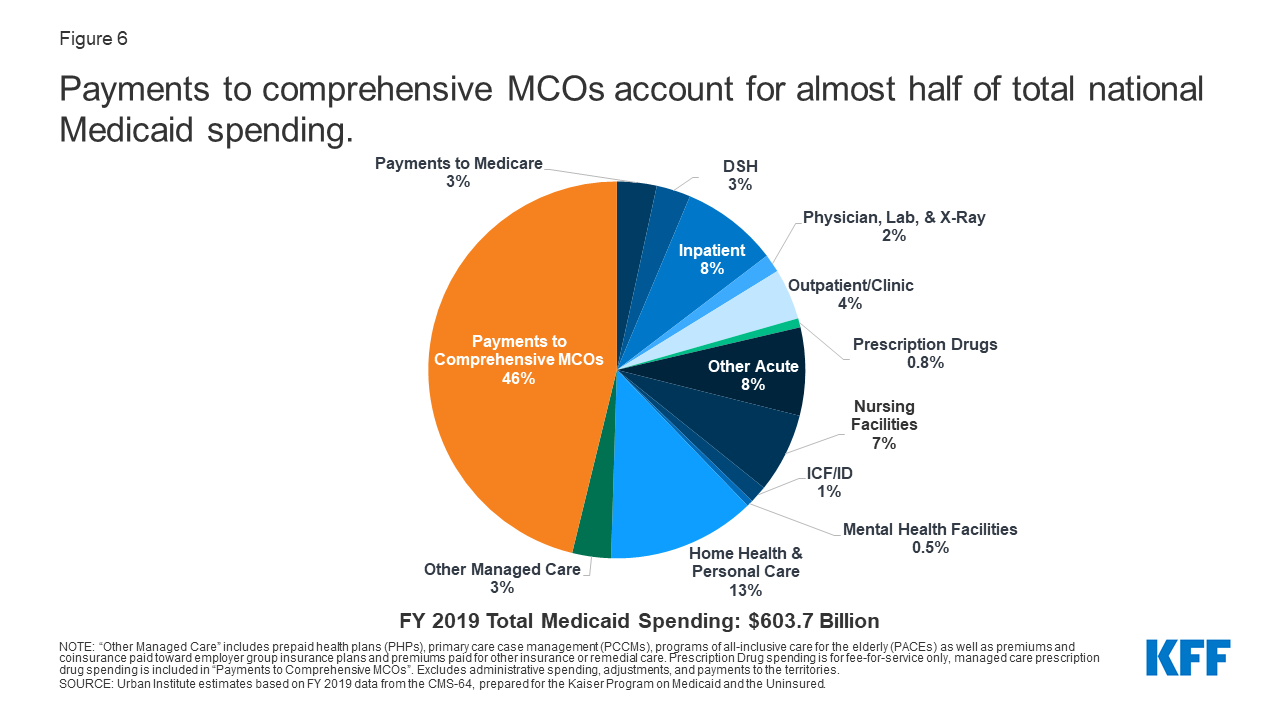
Medicaid managed care provides for the delivery of Medicaid health benefits and additional services through contracted arrangements between state Medicaid agencies and managed care organizations MCOs that accept a set per member per month capitation payment for these services. Conclusion Chronic disease is the leading cause of death which is costly and considered to be preventable Managed care organizations are implementing disease management programs to prevent chronic disease Risk factors such as tobacco use inactivity poor nutrition and excessive alcohol consumption should be resolved Smoking cessation programs will be successful with the. Managed care plans are a cost-effective use of health care resources that improve health care access and assure quality of care.
There are three primary types of managed care organizations. The overall goals of provider and member clinical and educational programs in managed care pharmacy are to maintain a high quality of care and reduce overall health care costsThis module discusses the role and use of clinical and educational programs pharmacy for providers and patients. History of managed care.
If you refer yourself to a provider outside the. Comprehensive risk-based health plans primary care case management programs and limited-benefit plans. A New Managed Care Program Contract in 2019 In October of 2019 a new 3-year contract went into effect with MCOs Mercy Care and UnitedHealthcare Community Plan UHCCP.
PPOs are by far the. Participating plans plan section and rate setting quality and performance incentives if the state programs are regulated and measured by HEDIS CAHPS etc. Managed Care is a health care delivery system organized to manage cost utilization and quality.
Compare and contrast managed care programs between two states. Learn more about Medicaid managed care payment.
 10 Things To Know About Medicaid Managed Care Kff
10 Things To Know About Medicaid Managed Care Kff
 What Is Managed Care The Motley Fool
What Is Managed Care The Motley Fool
 Managed Care Pharmacy 101 Amcp Org
Managed Care Pharmacy 101 Amcp Org
 Managed Care Programs Momoka Ito And Yui Nakajima 9781604564891 Amazon Com Books
Managed Care Programs Momoka Ito And Yui Nakajima 9781604564891 Amazon Com Books
 Exploring The Growth Of Medicaid Managed Care Congressional Budget Office
Exploring The Growth Of Medicaid Managed Care Congressional Budget Office
 Medicaid And Medicare Managed Care Programs In New York Download Table
Medicaid And Medicare Managed Care Programs In New York Download Table
 10 Things To Know About Medicaid Managed Care Kff
10 Things To Know About Medicaid Managed Care Kff
 How Can Managed Care Work For The I Dd Population Arlington Heritage Group Inc
How Can Managed Care Work For The I Dd Population Arlington Heritage Group Inc
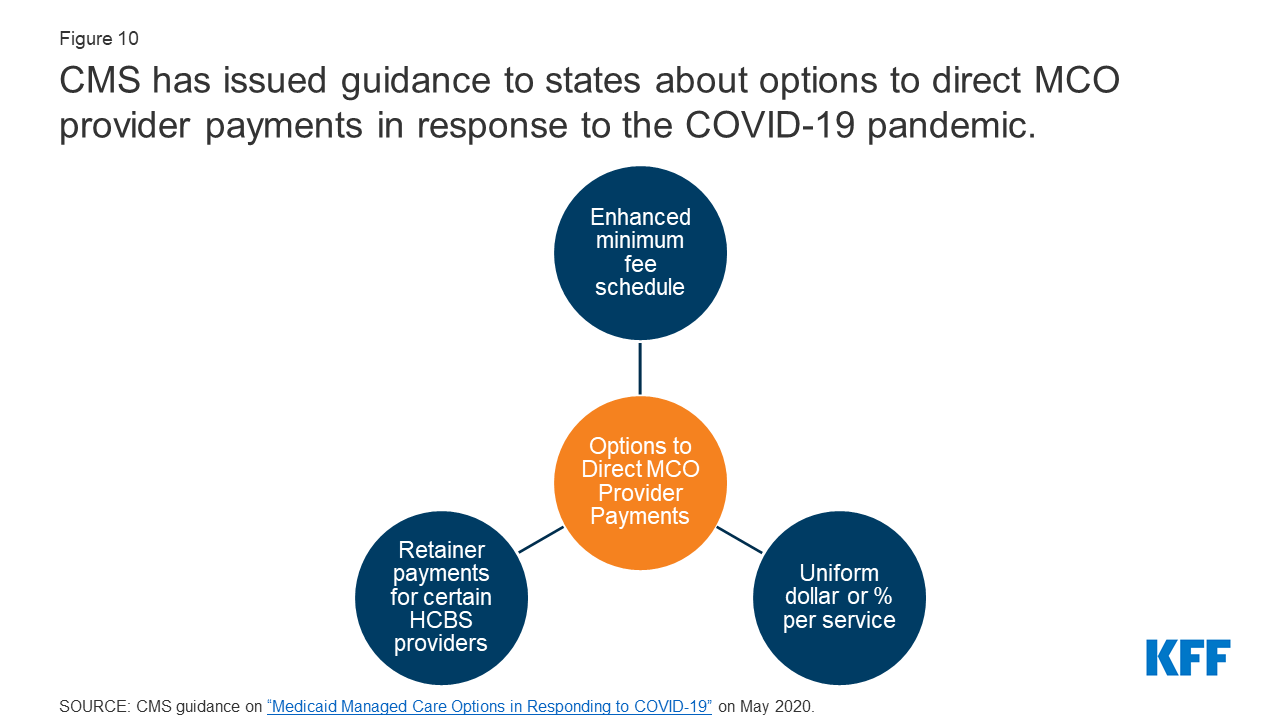 10 Things To Know About Medicaid Managed Care Kff
10 Things To Know About Medicaid Managed Care Kff
 Managed Care Images Page 1 Line 17qq Com
Managed Care Images Page 1 Line 17qq Com
 The Medicaid Managed Care Rule The Major Challenges States Face Commonwealth Fund
The Medicaid Managed Care Rule The Major Challenges States Face Commonwealth Fund
 What Is Managed Care The Motley Fool
What Is Managed Care The Motley Fool
 The History Of Managed Care Organizations In The United States Presentation Developed For The Academy Of Managed Care Pharmacy Updated February Ppt Download
The History Of Managed Care Organizations In The United States Presentation Developed For The Academy Of Managed Care Pharmacy Updated February Ppt Download


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.